COVID-19: Diagnostics, Treatments, and Long-Term Solutions
The first infection by the agent of COVID-19, variously called 2019-nCoV or SARS-CoV-2, probably happened around December 12, 2019, based on the interviews in late December with a group of new pneumonia patients in Wuhan, China. Most of the pneumonia cases turned out to be traceable, either directly or indirectly, to the city’s Huanan seafood market: a wholesale market that sold, not only seafood, but also wildlife like snakes, birds, marmots, bats, and probably also pangolins. The market was shut down and decontaminated on January 1. Nevertheless, within a week, China had 15 new infections. By then, Chinese scientists knew they were dealing with a new coronavirus. From that point on, they and health authorities have been extremely candid with the world about the status of the disease within their borders. Furthermore, China’s scientists quickly rose to the challenges of this new disease and in the process showed themselves to be the undisputed world leaders in coronavirus research.

The day the first patient died in China, on January 10, the first sequence of the virus’ genetic material, i.e. its genome sequence, was released online for all the world’s scientists to examine. The genome information was critical, because it made diagnosis for the virus possible for any molecular biology laboratory, or public health department, in any country. Thus we learned that, by January 24, the disease had already spread to 10 other countries by air travel. In China itself, it had spread to 25 other provinces, the number of identified cases had grown to more than 870, and the death toll had climbed to 26. By March 19, COVID-19 was a pandemic that had reached 242,000 people in more than 140 countries and killed 10,000.

Challenges posed by COVID-19
It became clear almost immediately that there had to be human-to-human transmission of the agent of COVID-19, because many of those infected, especially the air travelers, had never visited the Huanan market. This mode of transmission was shown rigorously in a very thorough paper in The Lancet on January 24. Now we also know that, as often occurs with coronavirus infections, the severity of the disease depends on the condition of the human infected. Compared to people younger than 39 years old, the fatality rate is 18-fold higher for those between 60 and 69; 40-fold higher for those between 70 and 79; and 70-fold higher for those over 80 years old. The increased vulnerability with age may be explained by the fact that, as our immune system ages, it tends to overreact. It is often this overreaction that kills. The fatality rates based on age are multiplied 3.5 times for people with cancer, 2.6 times for those with respiratory or cardiovascular disease, and 1.6 times for those with diabetes. For example, compared to a healthy 39-year old, a 60-year old with respiratory problems is almost 50 times more likely to die from COVID-19. It should be noted that in the United States, about 60 percent of adults suffer from those health problems.

COVID-19 is less lethal than SARS and much less so than MERS. But with the COVID-19 agent, the beta-coronaviruses seem to have learned to target every human frailty, even at the societal level. In children, who are continuously touched and coddled by human societies, the infections are asymptomatic but transmissible. Healthy and at-risk adults might eventually show symptoms, but the healthy adults may be infectious for 20 days without showing any sign of illness. It is even possible that some people are “super-spreaders” who can more easily cause infections: a well-known phenomenon with viral respiratory diseases. As social animals, we are now forced to isolate ourselves from each other because, if the virus is aerosolized in an enclosed space by somebody’s cough or sneeze, it will not disappear from the air until after 11 hours! It will not die on copper surfaces until after 8 hours, cardboard surfaces until 1 ½ day, stainless steel until 2 days, and plastic until 3 days.

In the virus’ crosshairs are the most powerful members of our society, including those who promote runaway growth and destruction of wildlife habitats. They tend to be over 60, and the association of their Western lifestyle with certain illnesses puts them at yet greater risk. In the US, there has been a reluctance to test for COVID-19 and quarantine those infected. At least one reason for this is that COVID-19 left China as an infection of middle and upper class intercontinental business travelers. In such a highly litigious society, rich asymptomatic politicians and businessmen were treated with deference, and not tested or quarantined, as they entered various airports in early to mid January bringing with them a pandemic.

Diagnoses
Drive-through ELISAs. South Korean scientists and others recently rolled out a relatively inexpensive (~ $7) and rapid color test to detect if a person’s immune system has produced antibodies against SARS-CoV-2 spike protein. This test is called an enzyme-linked immunosorbent assay, or ELISA. It can be done at home or in a drive-through setting in less than 5 minutes. A positive result means that you have been, at some time, exposed to the virus. It cannot tell your load of virus. In other words, if you show no symptom of disease, the test cannot tell if you are infectious and in the early stages of the disease, or if you have encountered the virus, completely cleared it, and recovered.

There should be no stigma or panic attached to a positive ELISA test result, which merely indicates a memory of the virus. A broad administration of such a test would greatly increase our understanding of the epidemiology of the infection. In this regard, it is encouraging that areas like New York State and San Antonio, Texas, are adopting the drive-through testing method. This will create an artificial spike in the number of US cases, but those cases are merely being exposed, and many of them have come and gone.

Real-time RT-PCR. Unlike ELISAs, which check our immune system’s memory of the virus, real-time RT-PCR directly tests for the virus. In the real-time RT-PCR test, one or more regions of the viral RNA collected from patients are iteratively doubled. A positive is considered to be a heavy load of virus that is detectable after few doublings (usually 37 or fewer, depending on the conditions), whereas a negative is taken as a failure to detect the virus after at least three additional doublings. This test is more expensive and slower than ELISAs.

Battery of tests. Chinese clinicians have cautioned that a 100 percent accurate diagnosis for COVID-19 requires a combination of criteria, including shortness of breath in a patient, a finding of lung lower-lobe pneumonia by CT scan of the chest, together with a positive result by real-time RT-PCR, plus fever, and a precipitous drop of certain types of white-blood cells. Alone, the ELISAs are 70 to 75 accurate, the CT scans are 90 percent accurate, and the real-time RT-PCR tests are 77 percent accurate. Real-time RT-PCR is the test promoted by the Centers for Disease Control and Prevention (CDC) in the US. In addition, the CDC has been requiring sequencing of the complete RNA genome of the virus from every patient: an expensive procedure that does not add to the diagnosis but monitors the virus’ evolution.

Containment of COVID-19. Given the above considerations, a logical approach for the containment of COVID-19 is to require:
- Mandatory ELISA tests for everyone and self-isolation for 20 days after a positive test.
- A battery of diagnostics for those who show early signs of the illness, starting with a CT scan, especially if they are over 60 years old or suffer from chronic health problems.
- Immediate isolation of all those who have come into contact with a COVID-19 patient.
- A careful record of all those who have recovered from an infection, because plasma donations from these individuals (discussed below) might in future save many lives.
- In addition to the usual hygiene recommendations, I would advise the following:
- Avoid indoor public spaces, and if you must be in such spaces and you have a choice, make only early morning visits.
- Use dilute Clorox, 1/3 cup of the bleach per gallon of water, to disinfect surfaces that have been handled by many people. Do not use antibacterial gels.
- Drink your liquids hot and eat lots of hot soups. The virus is easily killed at the temperatures of hot tea and coffee.

Treatments
With regard to treatments, we cannot hope for some silver bullet from scientists. The agent of COVID-19, like all other coronaviruses, has an error-prone reverse transcriptase that makes an average of 3 mistakes in every copy of virus. So these viruses have a potential for great genetic diversity and rapid change in the face of any kind of pressure. To control RNA viruses, usually a combination of several highly effective drugs is required, as is used against HIV. In the face of such a combination, a virus gains no advantage from accidentally learning not to respond to one drug, because the other drugs in the cocktail will still kill it. A virus – particularly an RNA virus — cannot be vanquished by attack at a single point: it must be assailed from all sides. Furthermore, regardless of the methods used to clear the virus that causes COVID-19, supportive care is essential. Therefore new facilities are needed for the treatment of patients during this pandemic.

Hydoxychloroquine. On March 18, an article in the scientific journal Cell Discovery showed that the inexpensive and widely available drug hydroxychloroquine (HCQ, trade name Plaquenil) can stop the in vitro infection of cultured monkey kidney cells by SARS-CoV-2. This drug is already being widely used to treat autoimmune disorders like lupus and rheumatoid arthritis. Hydroxychloroquine is related to chloroquine (CQ), which has been used to treat malaria. Chloroquine also works against SARS-CoV-2. Though its mechanism of action against the virus is as yet unknown, it is definitely not the same as that of its containment of the malarial parasite. The drug appears to prevent a movement of the virus from one compartment of the cells to another, which is required for the infection to proceed. Compared to CQ, HCQ is less potent against the virus; but HCQ is much safer, with fewer side effects. Since HCQ is readily absorbed by humans and much of it reaches the lung, liver, spleen, and kidney, the authors estimate that a safe dosage might be 6.0 to 6.5 milligrams per kilogram of body weight per day (approximately 400 to 450 milligrams daily for a 150-pound person), and they caution that “prolonged and overdose usage can still cause poisoning.”

Overnight, the world became greatly excited about these former malaria and arthritis drugs, and this enthusiasm is fueling initiatives to start major drug trials involving the use of HCQ against COVID-19 without delay. But this could actually make things worse. An extremely important and much overlooked observation by the researchers who wrote the article is that the HCQ-exposed viruses were evolving and becoming more infectious even during the experiments! Their words: this was “likely due to the adaptation of the virus in cell culture that significantly increased viral infectivity upon continuous passaging.”
Looking back at our abuse of antibiotics, I am sure that, given our current problems with hospital-acquired infections and flare-ups of antibiotic resistant bacterial pathogens throughout the world, we all wish we could have been more judicious with the use of such drugs. This experience should have taught us to approach our response to viruses with greater intelligence. Despite the raging pandemic, it would be prudent to wait to find another drug that kills the virus by a different mechanism and then always use a drug combination for any drug trial. If we do not do this, I predict that the drug trials using HCQ, on its own, will soon generate HCQ-resistant SARS-CoV-2 and a more lethal version of COVID-19.

Combination of hydroxychloroquine with azithromycin. In a paper accepted on February 27 by the International Journal of Antimicrobial Agents, though surprisingly not in press until March 17 and still not yet in final form online, Dr. Didier Raoult’s research group in Marseille, France, showed that the combination of hydroxychloroquine with azithromycin cleared the virus in six days. Hydroxychloroquine, trade name Plaquenil, is taken by mouth, has been in use since 1955 and costs $0.80 per 200-milligram pill. Azithromycin, trade name Zithromax or Z-Pak, is taken by mouth or intravenously; it has been in use since 1981 and costs $1.20 for a 250-milligram pill. Under no circumstance should anyone take any of the above drugs, which must first be prescribed, without consulting with a doctor.
Dr. Raoult’s study was extremely important, though admittedly small. It involved 36 individuals who were positive for SARS-CoV-2 with heavy loads of virus. Some were without symptoms, some had upper respiratory tract infections, and others had pneumonia. One group received 200 milligrams of Plaquenil three times daily, and another received Plaquenil and Zithromax. The patients who also received Zithromax got 500 milligrams on day 1, followed by 250 milligrams on subsequent days. Apart from hydroxychloroquine’s (Plaquenil) direct effect on the virus, described above, it is a well-established anti-inflammatory drug that is given, not only to lupus and arthritis patients, but also to patients with heavy microbial infections, to prevent their immune systems from overreacting in ways that might become lethal. Azithromycin (Zithromax) is an antibiotic that is sometimes given to patients to prevent secondary infections by bacteria, but there are signs that this drug might also work against a broad spectrum of viruses by some unknown mechanism.
The researchers monitored the patients daily for the viral loads deep in their nostrils (nasopharyngeal area) by real time RT-PCR, and the concentrations of the drug(s) in their sera. The controls were a group of similar patients who did not participate in the drug trial. By day 6, only 12.5 percent of the control group and 57 percent of the hydroxychloroquine-only group were virus free. By contrast, 100 percent of hydroxychloroquine-azithromycin patients were completely free of the virus after six days. This is an extraordinary result that deserves further study.

Convalescent plasma. One quite natural substance that attacks a virus from every possible side is convalescent plasma: the part of the blood of a former patient that is rich in antibodies against the recently defeated virus. The use of convalescent plasma is an old-fashioned low-tech approach that is applicable to most viral epidemics or pandemics, involves no severe adverse effects, but requires transparency and generosity. For this approach to work, we must identify the survivors of the viral infection, and they must willingly donate their plasma to help save others. Are we up to this task?
Blood transfusions from immune individuals of the same blood type as a patient is so far the only treatment that works against Ebola virus disease outbreaks. African scientists from Kinshasa University in the Democratic Republic of the Congo discovered this approach and published it in 1995 in the Journal of Infectious Diseases, and the WHO has approved its use during outbreaks. In Texas, in October 2014, a Dallas nurse was saved by a transfusion from Dr. Kent Brantly, who had himself been saved by a blood transfusion from a recovered 14-year old African Ebola patient. Nevertheless, questionable vaccines continue to be promoted for Ebola, and Ebola patients are even transported to the US for treatment, well away from the places where there exist many immune donors. These patients usually die.
Convalescent plasma does not require that the donor and patient be of the same blood type, because all the cells are removed from the blood that is donated by recovered patients. This treatment strategy has previously improved the survival rate of patients with SARS, as well as shortened their hospital stays. Treatment with convalescent plasma from the flu survivors apparently even reduced the fatality rate during the big 1918 influenza pandemic! The reason this approach is so effective is because the antibodies from the plasma bind to multiple parts of a virus and usher it to its destruction. Furthermore, these antibodies often attack, not only the free viruses, but also the infected human cells!
In mid-February, China issued a call for recovered COVID-19 patients to donate plasma. A State-owned Chinese company, called China National Biotec Group (CNBG) is responsible for testing and treating the plasma before it gets used. It should not surprise us at all that the number of Chinese daily fatalities has since greatly dropped. On March 19, the number of new deaths in China from COVID-19 was eight persons. The Japanese pharmaceutical giant, Takeda, announced on March 4 that it is initiating the manufacture of a plasma-derived product for COVID-19 called TAK-888. This will be done in Georgia, with US partners, and probably also in Asia and Europe. Transparency and generosity should be our guides during these difficult times, not jingoism and finger pointing.

The long term
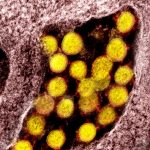
The solutions discussed above are for the short term. In future, we may expect recurrent coronavirus pandemics as well as new viruses, perhaps even multiple ones simultaneously, if we continue along the same path. It appears that we have been offered a preview of how our species might extinguish. Our nemeses are not the giant monsters that we create for our entertainment, but microscopic spheres of RNA, fat and protein, about 0.0001 millimeter wide, which are considered by some not even to be alive. For the long term, while we are at home, employed, unemployed, or quarantined, with plenty of time to consider our predicament, we must seriously rethink our treatment of other animals. The world needs to do an intense surveillance of animals for coronaviruses. We need to treat, not only human and livestock infections, but also wildlife infections. In addition, to be blunt about this, more of us need to adopt a vegetarian or vegan lifestyle. A major lesson from this episode is that when live bats, snakes, pangolins, civets, and raccoon dogs are being marketed wholesale somewhere for use by restaurants, this is not merely a cultural quirk that we should ignore. It is cruel. When Indonesia and the Amazon are being deforested, or even a nearby piece of wild land is being “developed” in anticipation of an ever-growing human population, we must respond passionately and quickly to these insults. Whether or not we want to accept the responsibility, it is ours. It is the business of every one of us, near and far, to stop these practices.

Editor’s Notes: Dr. Dady Chery is an Associate Professor of Biology, Editor of Haiti Chery, and the author of We Have Dared to Be Free: Haiti’s Struggle Against Occupation. Photographs one, three, six, ten and twelve from the Hospital Clinic de Barcelona archive; photographs two, eight, eleven, and fifteen from the NIH (National Institutes of Health); photographs four, five, nine and thirteen from the archive of New York National Guard; photograph sixteen by Meredith Nutting; and photograph seven from Dipartimento Protezione Civile.
Sources: Dady Chery | News Junkie Post.
Listen to a live interview of Dr. Dady Chery with hosts Bob Schlehuber and Jamarl Thomas of Radio Sputnik’s Political Misfits, on March 24, 2020.
Listen to “Don’t Panic But Do Act” on Spreaker.